In a world where medical breakthroughs are wiping out diseases left and right, cancer remains a stubborn killer that claims millions of lives each year. But a revolutionary breakthrough in gut health and cancer treatment is changing the game: immunotherapy that harnesses this powerful connection is offering fresh hope to patients battling the most stubborn forms of the disease.
The Microbiome Mystery: Why Some Patients Respond and Others Don’t
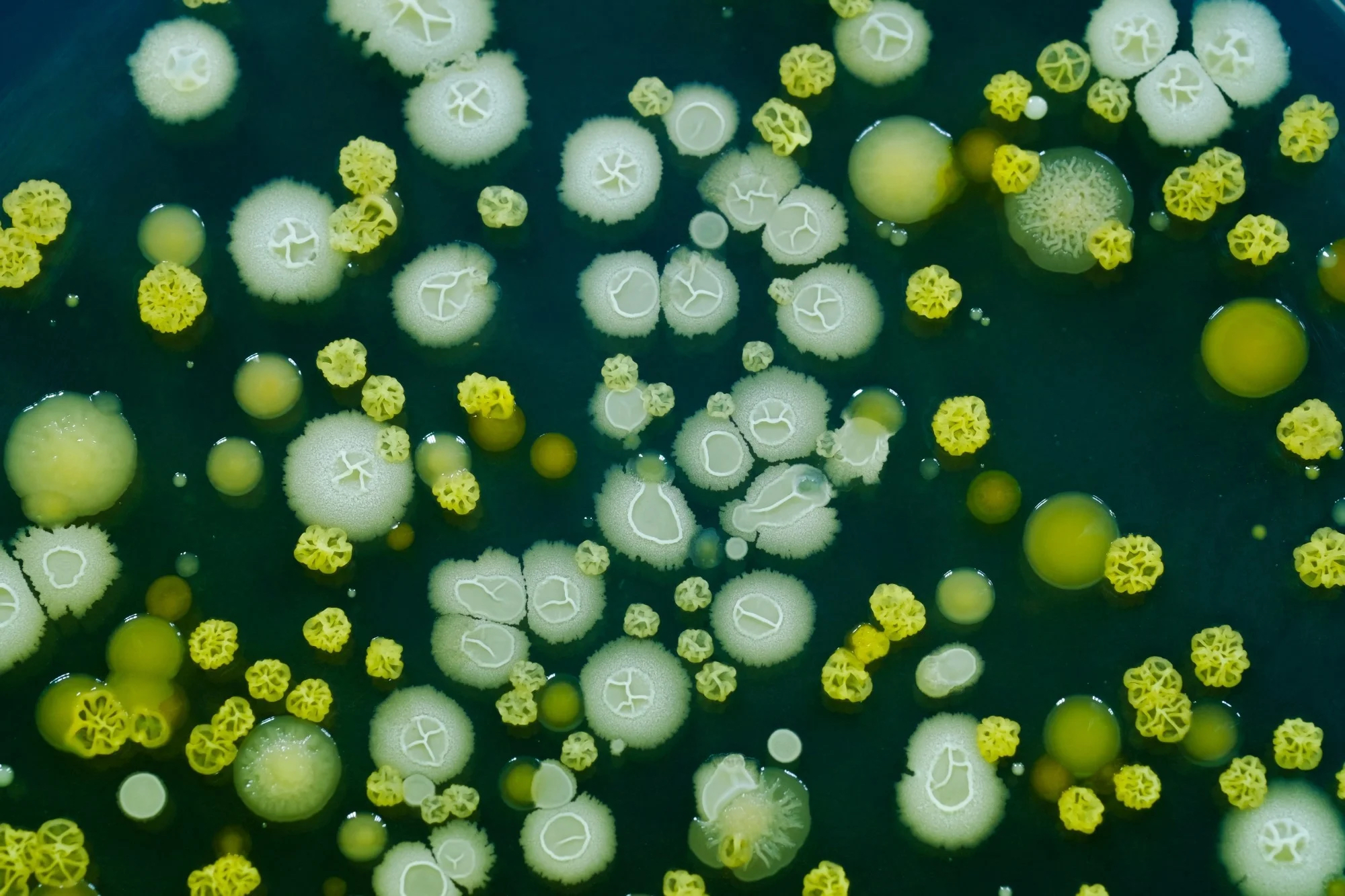
Tumor cells are able to fool our own immune system and prevent our body from attacking them. Immunotherapy releases this break from our immune system, allowing patients to battle the disease. However, even though immunotherapy has increased survival rates of cancer patients immensely, not all respond to this type of drug (2) . Consequently, researchers could not help but wonder: Could microbes in the gut be the ones to blame?
The answer is yes. Resistance to a type of cancer immunotherapy is attributed to abnormal gut microbiome composition, a new research published in the journal Science shows3.
The Akkermansia Advantage: One Bacteria That Could Change Everything
Routy and colleagues performed a study including patients suffering from lung, kidney or bladder cancer. They separated patients into groups of responders and non-responders to a specific type of immunotherapy, called PD-1 blockade, and tested their gut microbiome composition. A substantial 69% of responders, as well as 58 % of patients with a stable condition, had great amounts of the bacteria Akkermansia muciniphila, while it was only found in 34% of non-responders or patients who eventually died of the disease. These results show that specific types of bacteria could be linked to the beneficial effects of anti-tumor therapies.
From Lab to Life: Can We Transfer “Good” Gut Bacteria to Save Lives?
So, if the bacteria in our gut are responsible for these great benefits, could we give a nice, big scoop of the “good” bacteria to non-responding patients and turn them into responders? The researchers addressed this question using mouse-models of cancer. They took stool samples from responding and non-responding patients and put these “good” or “bad” gut bacteria into mice with tumors. When they were subsequently treated with immunotherapy, mice that received “good” bacteria responded to the treatment, while mice with “bad” bacteria did not. Interestingly, when the researchers enriched the “bad” bacteria with Akkermansia muciniphila (the species that was found abundant in the responding patients) mice that were non-responders started to be sensitive to immunotherapy. Whether these promising results could be translated into human clinical studies remains to be resolved.
The Antibiotic Paradox: When Infection Treatment Hurts Cancer Care
Given that microbes are such crucial players in the fight against cancer, it is not surprising that the researchers found that antibiotics influence this process as well (3). They studied patients with bladder or lung cancer who received antibiotics for common infections, 2 months before or 1 month after their first treatment with PD-1 blockade immunotherapy. The research showed that these patients had markedly shorter survival rates, compared to patients that did not receive any antibiotics.
The presence of specific microbes, such as types of Escherichia coli, produce enzymes that inactivate certain anti-tumor drugs.
However, one should be careful when considering the negative effects of antibiotics on cancer treatment. It has been shown that the presence of specific microbes, such as types of Escherichia coli, produce enzymes that inactivate certain anti-tumor drugs (4) . This finding invites the possibility that the combination of antibiotic treatment with cancer therapy might also be beneficial.
Precision Medicine Gets Personal: Your Gut as Your Treatment Guide
As a take-home message, Christian Jobin, Ph.D., of the University of Florida, wrote in the editorial that was published along Routy’s research in Science: “The presence of specific strains of bacteria may be able to modulate cancer progression and therapeutics, raising the possibility that precision medicine directed at the microbiota could inform physicians about prognosis and therapy.” (5)