Among the superstars of the gut microbiome, Roseburia is one core genus that can be found in all populations of the world. Often used as a marker for good health, read on to find out how Roseburia supports your immune system and helps your gut feel its best!
Unlike its more famous counterparts Lactobacillus and Bifidobacteria, Roseburia is one genus of bacteria that is slightly less represented, yet still plays a major role in the gut microbiome. This core genus is represented in populations all over the world, making up between 3-15% of the total bacterial count in a healthy gut1.
The Roseburia genus comprises five important species: Roseburia intestinalis, R. hominis, R. inulinivorans, R. faecis, and R. cecicola. These bacteria are also thought to play an important role in colonizing the gut after birth. Studies have found that Roseburia were not present in the gut microbiomes of newborns but likely acquired through the consumption of breast milk, in which Roseburia can be found2. Meanwhile, following colonization of the gut, Roseburia counts have been shown to decline with age3.
Roseburia functions as an important butyrate producer to generate energy
In the body, Roseburia secretes various molecules that then interact with the host and other bacteria in the gut. These include short chain fatty acids (SCFAs) such as acetate, propionate and butyrate, which are produced after the fermentation, or breaking down, of indigestible dietary carbohydrates (e.g. plant fibres)4.
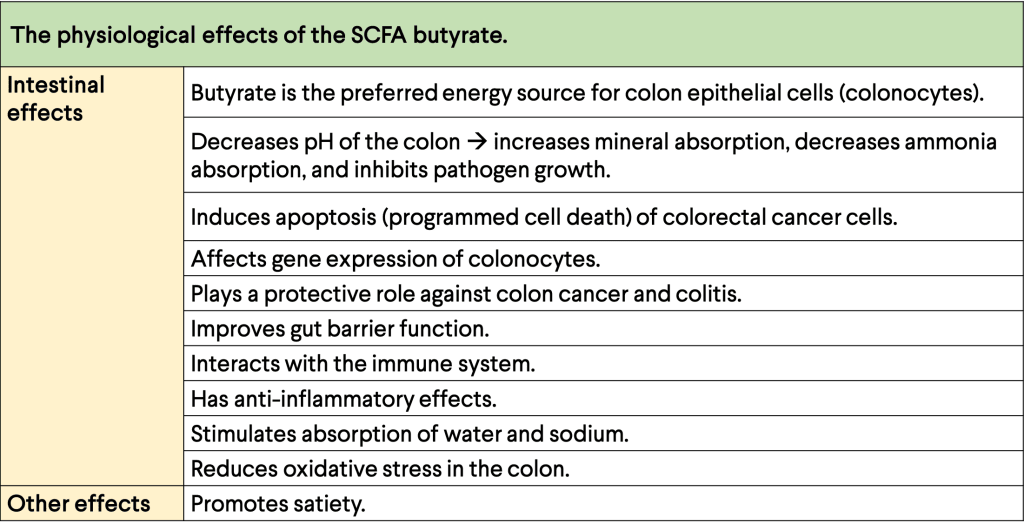
SCFAs are produced by the friendly bacteria in the gut and play important roles in health and disease, as well as in the metabolism of important nutrients such as carbohydrates and fats. They work to ensure that the intestine functions as normal and regulates the immune system through their anti-inflammatory properties1.
Butyrate is a key factor in the interactions between us and Roseburia.
Roseburia particularly prefers to produce high levels of the SCFA butyrate. These compounds are typically involved in energy generation and have been shown to protect the gut against pathogens and diseases, amongst other things5. This feature suggests that butyrate is a key factor in the interactions between us and Roseburia.
How your diet influences the Roseburia in your gut
Diet is a major influencer of the gut microbiome. The Mediterranean diet, which includes primarily plant-based foods (e.g. fruit and vegetables), whole grains, legumes and nuts, has long been associated with many health-improving properties6, and is particularly associated with higher levels of Roseburia species in the gut7. The reason for this is that dietary carbohydrates in the Mediterranean diet and other plant-based diets particularly favour the growth of certain butyrate-producing bacteria such as Roseburia.
Furthermore, the pH in the gut also affects the composition of the gut microbiota8. The acidic environment created in the gut after fermenting dietary carbohydrates can be beneficial as acidity can inhibit the growth of harmful microorganisms9. Butyrate levels are also higher with a more acidic gut environment (~pH 5.5), and this is linked to your microbiome’s composition – more Roseburia in the gut induces more carbohydrate fermentation, thereby lowering the pH and promoting the production of butyrate10.
Roseburia levels in the gut is often linked to good health
Anti-inflammatory properties
SCFAs such as butyrate produced by Roseburia are the main source of energy for epithelial cells in the gut called colonocytes, which promotes the control of inflammatory properties in the gut1.
Gut health
Many studies have found a link between Roseburia and gut health, including IBD, IBS, and colon cancer. Those affected with IBD, specifically ulcerative colitis (UC) and Crohn’s disease (CD), have shown a significant decrease in butyrate-producing bacteria, importantly Roseburia species. Fewer Roseburia in those affected with UC has also been correlated with reduced SCFA concentrations, consequently impairing butyrate and thus energy supply to anti-inflammatory colonocytes11. In patients with CD, the lack of Roseburia has been reported to be a specific change in the gut microbiome12.
Similarly, lower Roseburia populations in the gut microbiomes of patients with IBS lead to lower butyrate production and hence alter carbohydrate metabolism. Overall, this dysbiosis is linked to higher incidence of IBS symptoms, including diarrhoea and constipation12.
Colorecatal cancer has also been associated with changes in the gut microbiome involving a decrease in Roseburia populations, as it has been observed that increased butyrate production by gut bacteria can be linked to reduced incidence of colon cancer13.
Obesity & diabetes
Studies in both mice and humans show that Roseburia species are much lower compared to leaner subjects14. In one study, a group of obese subjects who received faecal transplants from lean donors resulted in beneficial metabolic effects as well as significantly higher diversity in the microbiome, including distinct levels of butyrate-producers such as Roseburia15.
Roseburia is also lacking in the microbiomes of patients with Type 2 diabetes compared with healthy subjects; Roseburia negatively correlates with plasma glucose. Some scientists suggest that beneficial gut bacteria including Roseburia and Bifidobacteria work to regulate glucose levels and prevent progression into prediabetic/diabetic conditions16.
Other diseases
Various other diseases have also been linked to changes in the abundance of Roseburia. For example, lower abundance of Roseburia are associated with incidences of liver cirrhosis and hepatic encephalopathy1. It has also been suggested to play a protective role of the nervous system because of its association with lower incidence of neurological diseases such as Parkinson’s1.
Want to find out how the Roseburia levels in your gut shape up?
Certain foods can help you raise your levels of Roseburia (see Figure on left.) Many studies agree that Roseburia bacteria play a major role in maintaining gut health through the production of butyrate, and ensuring immune defence against nasty pathogens. Links between lower Roseburia levels and several intestinal disorders suggest that these beneficial bacteria is one to watch for when studying our gut health. Interested in how your gut microbiome shapes up? Check out our RESET program to get a snapshot of gut microbes, including those all-important butyrate producing Roseburia, followed by our full support on a successful gut intervention!